Using CSF dynamics recordings to change the neurosurgical care of hydrocephalic and IIH patients
Shunt testing in vivo: the importance and impact of the computerised CSF infusion test
CSF infusion tests in shunted individuals are critical in preventing unnecessary, blind revisions of shunts and provide evidence of shunt malfunction.
The CSF infusion test for shunt testing in vivo was developed after years of experience in the Cambridge Shunt Evaluation Laboratory; all of the shunt properties and the analysis of the CSF dynamics after shunting (for testing of the shunt function) are integrated into ICM+.
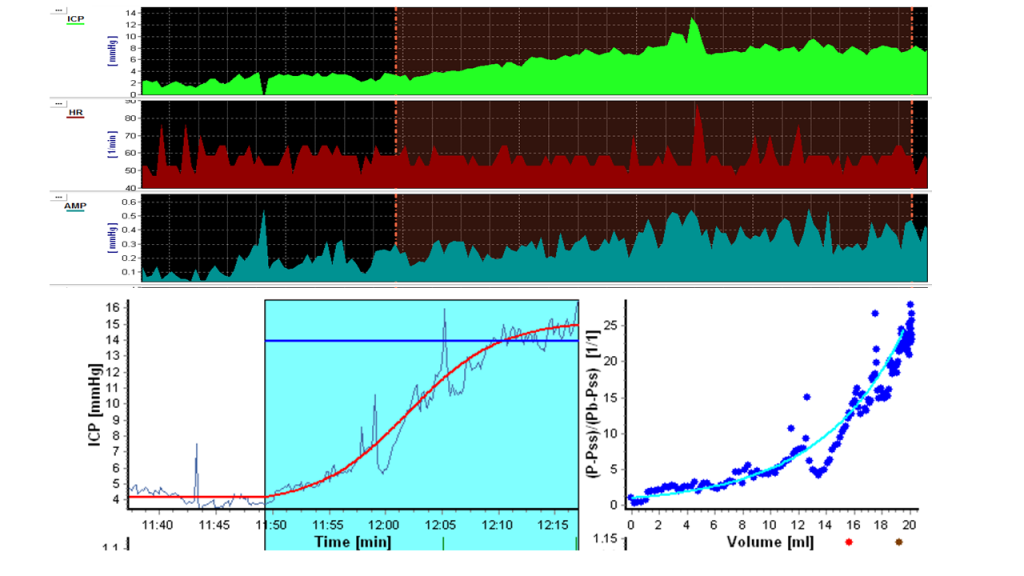
All the different shunt characteristics (shunt critical ICP, resistance etc) are incorporated in ICM+ and each patient can be assessed depending on the implanted valve and/or setting of the valve (strata/strata NSC, Orbis-Sigma etc). All the valves have been tested at the Cambridge shunt evaluation laboratory established >20 years ago View image

If the steady-state plateau ICP achieved after infusion does not exceed the shunt-critical ICP, then the valve is draining at least sufficiently (over-drainage needs to be excluded). If the ICP plateau exceeds the maximum value normally allowed by the shunt design and/or setting, then under-drainage or blockage should be suspected. View image
Impact of shunt testing in vivo on patient outcome
With subsequent financial benefit for the NHS
Measuring shunted patients’ CSF dynamics and assessing their shunt function in vivo is not only for research!
Shunt function test reporting is utilised by the clinical team to support the decision on whether or not to proceed to shunt revision, setting manipulation, or even reassure and manage the symptoms conservatively.
Out of an average of 120 infusion studies per year of both IIH and hydrocephalic individuals (of almost 100 different patients), only 14-16 patients have evidence of shunt blockage or other malfunction requiring revision or other neurosurgical intervention.
Of the remaining 104-106 patients available for follow up, > 80 (that is >75% total) remain symptom-free with either neurologic care for their headaches, adjustment of the setting, or reassurance.
IIH patients are the ones accounting for most of the non-improving patients, due to a more complex spectrum of clinical sympoms that are not always dependent on shunt malfunction. Almost all the non-improving hydrocephalic patients do not end up with a revision owing to shunt blockage.
Preventing unnecessary revisions is crucial for the patients’ future uncomplicated course and especially for the cognitive outcome and quality of life of paediatric patients.
It also helps the NHS significantly lower the costs of performing surgeries that could have been avoided.


